Table of Contents
Introduction
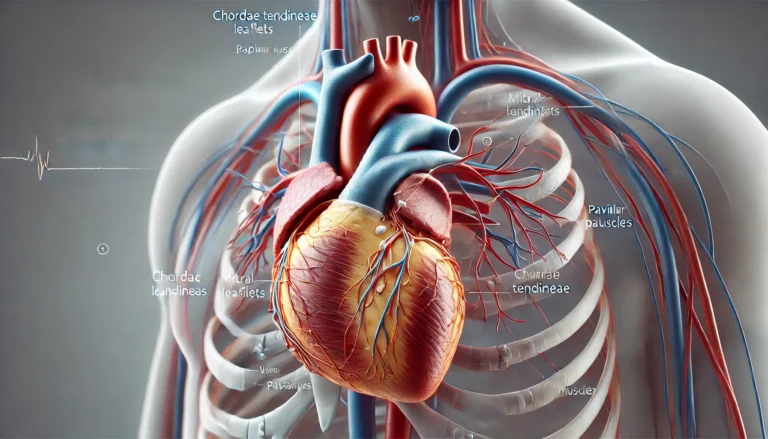
Chordae tendineae, often referred to as “heart strings,” are a critical component of the heart’s mitral and tricuspid valves. These fibrous cords connect the valve leaflets to the papillary muscles, playing a vital role in maintaining the proper function of the heart by ensuring valve closure during ventricular contraction. This article delves into the structure, function, and clinical significance of chordae tendineae, drawing on extensive research and clinical studies to provide a comprehensive overview.
Structure of Chordae Tendineae
Chordae tendineae are composed of dense connective tissue primarily made up of collagen, elastin, and glycosaminoglycans. These components confer the necessary strength and flexibility to withstand the mechanical stresses experienced during each cardiac cycle. The chordae can be classified into primary, secondary, and tertiary types based on their attachment and function (Lam et al., 1970).

Types of Chordae Tendineae
- Primary Chordae:
- Attach directly to the free edges of the valve leaflets.
- Crucial for preventing prolapse of the leaflets into the atrium during systole.
- Bear the most significant mechanical load.
- Secondary Chordae:
- Attach to the ventricular surface of the valve leaflets.
- Provide additional support to the valve apparatus.
- Tertiary Chordae:
- Attach to the ventricular wall.
- Ensure effective closure of the valve during ventricular contraction.
Composition of Chordae Tendineae
| Component | Function |
| Collagen | Provides tensile strength |
| Elastin | Offers elasticity and resilience |
| Glycosaminoglycans | Contribute to structural integrity and flexibility |
Function of Chordae Tendineae
The primary function of chordae tendineae is to anchor the valve leaflets to the papillary muscles, which contract during systole, pulling the chordae taut and preventing the inversion or prolapse of the valve leaflets. This mechanism ensures that the valves close properly, preventing the backflow of blood into the atria (Sanders et al., 1967).
Clinical Significance
The integrity and function of chordae tendineae are crucial for maintaining normal cardiac function. Various pathological conditions can affect these structures, leading to significant clinical implications.
Mitral Regurgitation
Mitral regurgitation is a condition where the mitral valve fails to close properly, allowing blood to flow backward into the left atrium. One common cause is the rupture of the chordae tendineae, which compromises the valve’s ability to seal effectively. Surgical repair techniques, such as chordal transfer and chordal replacement, have been developed to address this issue (Smedira et al., 1996).
Mitral Valve Prolapse
Mitral valve prolapse occurs when the valve leaflets bulge into the left atrium during systole. This condition is often associated with elongated or ruptured chordae tendineae. Repair strategies include the use of artificial chordae made from materials like expanded polytetrafluoroethylene (ePTFE) to restore proper valve function (Revuelta et al., 1989).
Tricuspid Valve Pathology
Similar to the mitral valve, the tricuspid valve can also suffer from chordae tendineae rupture, leading to tricuspid regurgitation. Repair of tricuspid valve involves techniques like chordal replacement to restore valve competency (Khoiy et al., 2018).

Rheumatic Heart Disease
Rheumatic heart disease can lead to thickening and fibrosis of the chordae tendineae, affecting their flexibility and strength. This can result in either stenosis or regurgitation of the valves, necessitating surgical intervention (Sanders et al., 1967).
Surgical Techniques and Innovations
Several surgical techniques have been developed to repair damaged chordae tendineae. These techniques aim to restore the structural integrity and function of the valves, ensuring effective blood flow and reducing the risk of complications.
Chordal Transfer and Chordal Replacement
Chordal transfer involves using intact chordae from other parts of the valve to replace the ruptured or elongated chordae. Chordal replacement uses synthetic materials like ePTFE sutures to recreate the function of the natural chordae. Studies have shown that chordal transfer is often superior to chordal shortening in terms of long-term outcomes (Phillips et al., 2000).
Artificial Chordae
The use of artificial chordae, such as those made from ePTFE, has revolutionized valve repair techniques. These synthetic materials mimic the mechanical properties of natural chordae and provide a durable solution for patients with ruptured chordae tendineae (Salvador et al., 2008).
NeoChord Procedure
The NeoChord procedure is a minimally invasive technique that involves the placement of artificial chordae tendineae through a small incision, avoiding the need for open-heart surgery. This procedure has shown promising results in terms of safety and efficacy, providing a less invasive option for patients with mitral valve prolapse (Colli et al., 2015).
Transcatheter Techniques
Emerging transcatheter techniques aim to repair chordae tendineae without the need for open surgery. These techniques involve the delivery of artificial chordae or other supportive structures via catheterization, potentially reducing recovery times and complications associated with traditional surgical approaches (Tabata et al., 2014).
Biomechanical Properties and Research
Research into the biomechanical properties of chordae tendineae has provided valuable insights into their function and the impact of various repair techniques.
Viscoelastic Properties
Chordae tendineae exhibit viscoelastic properties, which allow them to absorb and dissipate the mechanical energy generated during the cardiac cycle. This viscoelasticity is crucial for their ability to withstand repetitive loading without undergoing permanent deformation (Cochran & Kuzelman, 1991).
Material Properties
Studies have compared the material properties of native chordae tendineae with those of synthetic materials used in chordal replacement. These studies help in optimizing the design of artificial chordae to closely match the performance of natural structures (Ritchie et al., 2005).
Fatigue and Failure Mechanics
Understanding the fatigue life and failure mechanics of chordae tendineae is essential for predicting their long-term performance, especially in patients undergoing valve repair with artificial chordae. Research in this area focuses on the modes of damage accumulation and the factors influencing fatigue life (Gunning & Murphy, 2016).
Stress-Strain Characteristics
Research has shown that chordae tendineae demonstrate specific stress-strain characteristics that are essential for their function. These properties ensure that the chordae can stretch and recoil without damage during the cardiac cycle (Lim & Boughner, 1975).
Influence of Aging

Aging affects the biomechanical properties of chordae tendineae, leading to changes in their elasticity and strength. Studies on aged human and animal models have provided insights into these changes and their implications for valve function (Zuo et al., 2016).
Mechanical Properties
| Property | Description |
| Tensile Strength | Ability to withstand pulling forces without breaking |
| Elastic Modulus | Measurement of elasticity, indicating how much a material will deform under stress |
| Fatigue Resistance | Ability to resist degradation over repeated cycles of stress and strain |
| Viscoelasticity | Combines viscous and elastic properties, allowing absorption and dissipation of energy |
| Stress-Strain Characteristics | Relationship between stress (force per unit area) and strain (deformation) under load |
Morphological Studies
Morphological studies of chordae tendineae provide detailed insights into their structural organization and variations.
Human Cadaveric Studies
Morphological studies on human cadaveric hearts have classified chordae tendineae based on their attachment points and structural characteristics. These studies form the basis for understanding the normal anatomy and variations that can occur in pathological conditions (Gunnal et al., 2015).
Read: What is Trabeculae Carnea?
Fetal Heart Studies
Research on fetal hearts has revealed the development and morphological features of chordae tendineae at different stages of gestation. This knowledge is crucial for understanding congenital heart defects and developing early intervention strategies (De Almeida et al., 2019).
Comparative Studies
Comparative studies between human and animal models, such as porcine hearts, provide valuable information on the similarities and differences in chordae tendineae structure and function. These studies are essential for developing animal models that accurately mimic human cardiac physiology (Crick et al., 1998).
Histological Analysis
Histological analysis of chordae tendineae involves examining the tissue at a microscopic level to understand its cellular composition and structural organization. These studies help identify pathological changes associated with various cardiac conditions (Lim et al., 1977).
Ultrastructure Studies
Ultrastructure studies using electron microscopy provide detailed images of the microstructure of chordae tendineae, revealing the organization of collagen fibers and other cellular components. These studies are crucial for understanding the mechanical properties of the tissue (Lim, 1980).
Morphological Characteristics
| Study Type | Key Findings |
| Human Cadaveric Studies | Classification of chordae based on attachment and structure |
| Fetal Heart Studies | Developmental features and congenital abnormalities |
| Comparative Studies | Similarities and differences between human and animal models |
| Histological Analysis | Cellular composition and structural organization |
| Ultrastructure Studies | Microstructural details and mechanical property correlations |
Advances in Imaging and Modeling
Advances in imaging and computational modeling have significantly enhanced our understanding of chordae tendineae and their role in valve mechanics.
Imaging Techniques
Modern imaging techniques, such as 3D echocardiography and MRI, allow for detailed visualization of chordae tendineae in vivo. These techniques provide real-time information on their motion and interactions with the valve leaflets, aiding in the diagnosis and planning of surgical interventions (Ionasec, 2010).
Finite Element Modeling
Finite element modeling is a powerful tool for simulating the mechanical behavior of chordae tendineae under different conditions. These models help in predicting the outcomes of various surgical techniques and optimizing the design of artificial chordae (Kunzelman et al., 1996).
Read: Curette and Endocervical Curettage (ECC)
Patient-Specific Models
Patient-specific models, derived from imaging data, enable personalized treatment planning by simulating the mechanical behavior of an individual’s chordae tendineae and valve leaflets. This approach allows for tailored surgical strategies that improve patient outcomes (Aggarwal et al., 2013).
Biomechanical Simulations
Biomechanical simulations using patient-specific data provide insights into the dynamic behavior of chordae tendineae during the cardiac cycle. These simulations help identify potential issues with valve function and guide surgical planning (Rim et al., 2014).
Advances in Imaging and Modeling
| Technique | Application |
| 3D Echocardiography | Real-time visualization of chordae and valve interactions |
| MRI | Detailed imaging of cardiac structures |
| Finite Element Modeling | Simulation of mechanical behavior under various conditions |
| Patient-Specific Models | Personalized treatment planning and surgical strategy optimization |
| Biomechanical Simulations | Analysis of dynamic behavior during the cardiac cycle |
Future Directions and Research
Ongoing research aims to further our understanding of chordae tendineae and improve clinical outcomes for patients with valve diseases.
Tissue Engineering
Tissue engineering approaches aim to create bioengineered chordae tendineae that can integrate with the patient’s native tissue and grow over time. These approaches hold promise for providing long-lasting solutions for valve repair (Madhurapantula et al., 2020).
Biomaterials
The development of new biomaterials that closely mimic the mechanical properties of natural chordae tendineae is a key area of research. These materials should be biocompatible, durable, and capable of withstanding the mechanical stresses of the cardiac cycle (Caimmi et al., 2016).
Genetic and Molecular Studies
Understanding the genetic and molecular basis of chordae tendineae development and pathology can provide insights into the mechanisms underlying valve diseases. This knowledge can lead to the identification of new therapeutic targets and the development of novel treatment strategies (Krishnamurthy & Grande-Allen, 2018).
Innovations in Surgical Techniques
Continued innovation in surgical techniques aims to improve the outcomes of valve repair procedures. Minimally invasive approaches and advanced imaging techniques are likely to play a significant role in the future of chordae tendineae repair (Siefert et al., 2014).
Long-term Outcomes
Long-term studies on the outcomes of various repair techniques are essential for understanding their effectiveness and durability. These studies will help refine surgical approaches and improve patient care (Tabata et al., 2014).
Read: What is Cystolitholapaxy?
Conclusion
Chordae tendineae are vital structures in the heart, ensuring the proper function of the mitral and tricuspid valves. Advances in surgical techniques, imaging, and biomechanical research have significantly improved our understanding and treatment of diseases affecting these structures. Ongoing research continues to explore innovative approaches to repair and replace damaged chordae tendineae, promising better outcomes for patients with valvular heart diseases.
REFERENCES
Sanders, C. A., Austen, W. G., Harthorne, J. W., Dinsmore, R. E., & Scannell, J. G. (1967). Diagnosis and surgical treatment of mitral regurgitation secondary to ruptured chordae tendineae. The New England Journal of Medicine, 276(16), 943–949.
Khoiy, K. A., Asgarian, K. T., Loth, F., & Amini, R. (2018). Dilation of tricuspid valve annulus immediately after rupture of chordae tendineae in ex-vivo porcine hearts. PLoS ONE, 13(11), e0206744.
Smedira, N. G., Selman, R., Cosgrove, D. M., McCarthy, P. M., Lytle, B. W., Taylor, P. C., Apperson-Hansen, C., Stewart, R. W., & Loop, F. D. (1996). Repair of anterior leaflet prolapse: Chordal transfer is superior to chordal shortening. The Journal of Thoracic and Cardiovascular Surgery, 112(2), 287–292.
Phillips, M. R., Daly, R. C., Schaff, H. V., Dearani, J. A., Mullany, C. J., & Orszulak, T. A. (2000). Repair of anterior leaflet mitral valve prolapse: Chordal replacement versus chordal shortening. The Annals of Thoracic Surgery, 69(1), 25–29.
Revuelta, J. M., Garcia-Rinaldi, R., Gaite, L., Val, F., & Garijo, F. (1989). Generation of chordae tendineae with polytetrafluoroethylene stents: Results of mitral valve chordal replacement in sheep. The Journal of Thoracic and Cardiovascular Surgery, 97(1), 98–103.
Tabata, M., Kasegawa, H., Fukui, T., Shimizu, A., Sato, Y., & Takanashi, S. (2014). Long-term outcomes of artificial chordal replacement with tourniquet technique in mitral valve repair: A single-center experience of 700 cases. The Journal of Thoracic and Cardiovascular Surgery, 148(5), 2033–2038.e1.
Cochran, R. P., & Kuzelman, K. S. (1991). Comparison of viscoelastic properties of suture versus porcine mitral valve chordae tendineae. Journal of Cardiac Surgery, 6(4), 508–513.
Colli, A., Manzan, E., Rucinskas, K., Janusauskas, V., Zucchetta, F., Zakarkaite, D., Aidietis, A., & Gerosa, G. (2015). Acute safety and efficacy of the NeoChord procedure. Interactive CardioVascular and Thoracic Surgery, 20(5), 575–581.
Gunnal, S. A., Wabale, R. N., & Farooqui, M. S. (2015). Morphological study of chordae tendineae in human cadaveric hearts. Heart Views: The Official Journal of the Gulf Heart Association, 16(1), 1–12.
Lam, J. H. C., Ranganathan, N., Wigle, E. D., & Silver, M. D. (1970). Morphology of the human mitral valve: I. Chordae tendineae: A new classification. Circulation, 41(3), 449–458.
Zuo, K., Pham, T., Li, K., Martin, C., He, Z., & Sun, W. (2016). Characterization of biomechanical properties of aged human and ovine mitral valve chordae tendineae. Journal of the Mechanical Behavior of Biomedical Materials, 62, 607–618.
De Almeida, M. T. B., Aragao, I. C. S. A., Aragao, F. M. S. A., Reis, F. P., & Aragao, J. A. (2019). Morphological study on mitral valve chordae tendineae in the hearts of human fetuses. International Journal of Anatomical Variations, 12(1), 17–20.
Salvador, L., Mirone, S., Bianchini, R., Regesta, T., Patelli, F., Minniti, G., … & Valfrè, C. (2008). A 20-year experience with mitral valve repair with artificial chordae in 608 patients. The Journal of thoracic and cardiovascular surgery, 135(6), 1280-1287.
Ritchie, J., Jimenez, J., He, Z., Sacks, M. S., & Yoganathan, A. P. (2006). The material properties of the native porcine mitral valve chordae tendineae: an in vitro investigation. Journal of biomechanics, 39(6), 1129-1135.
Gunning, G. M., & Murphy, B. P. (2016). The effects of decellularization and cross-linking techniques on the fatigue life and calcification of mitral valve chordae tendineae. Journal of the Mechanical Behavior of Biomedical Materials, 57, 321-333.
Lim, K. O., & Boughner, D. R. (1975). Mechanical properties of human mitral valve chordae tendineae: variation with size and strain rate. Canadian journal of physiology and pharmacology, 53(3), 330-339.
Crick, S. J., Sheppard, M. N., Ho, S. Y., Gebstein, L., & Anderson, R. H. (1998). Anatomy of the pig heart: comparisons with normal human cardiac structure. The Journal of Anatomy, 193(1), 105-119.
Lim, K. O., & Boughner, D. R. (1977). Scanning electron microscopical study of human mitral valve chordae tendineae. Archives of Pathology & Laboratory Medicine, 101(5), 236-238.
Lim, K. O. (1980). Mechanical properties and ultrastructure of normal human tricuspid valve chordae tendineae. The Japanese journal of physiology, 30(3), 455-464.
Ionasec, R. I. (2010). Patient-specific modeling and quantification of the heart valves from multimodal cardiac images (Doctoral dissertation, Technische Universität München).
Kunzelman, K. S., & Cochran, K. P. (1990). Mechanical properties of basal and marginal mitral valve chordae tendineae. ASAIO Journal, 36(3), M405-407.
Aggarwal, A., Aguilar, V. S., Lee, C. H., Ferrari, G., Gorman, J. H., Gorman, R. C., & Sacks, M. S. (2013). Patient-specific modeling of heart valves: from image to simulation. In Functional Imaging and Modeling of the Heart: 7th International Conference, FIMH 2013, London, UK, June 20-22, 2013. Proceedings 7 (pp. 141-149). Springer Berlin Heidelberg.
Rim, Y., Laing, S. T., McPherson, D. D., & Kim, H. (2014). Mitral valve repair using ePTFE sutures for ruptured mitral chordae tendineae: a computational simulation study. Annals of biomedical engineering, 42, 139-148.
Madhurapantula, R. S., Krell, G., Morfin, B., Roy, R., Lister, K., & Orgel, J. P. (2020). Advanced methodology and preliminary measurements of molecular and mechanical properties of heart valves under dynamic strain. International Journal of Molecular Sciences, 21(3), 763.
Caimmi, P. P., Sabbatini, M., Fusaro, L., Borrone, A., & Cannas, M. (2016). A study of the mechanical properties of ePTFE suture used as artificial mitral chordae. Journal of cardiac surgery, 31(8), 498-502.
Krishnamurthy, V. K., & Jane Grande-Allen, K. (2018). The role of proteoglycans and glycosaminoglycans in heart valve biomechanics. Advances in Heart Valve Biomechanics: Valvular Physiology, Mechanobiology, and Bioengineering, 59-79.
Siefert, A. W., Rabbah, J. P. M., Pierce, E. L., Kunzelman, K. S., & Yoganathan, A. P. (2014). Quantitative evaluation of annuloplasty on mitral valve chordae tendineae forces to supplement surgical planning model development. Cardiovascular engineering and technology, 5, 35-43.


Pingback: Back Throat Bumps 101: Causes, Diagnosis, and Treatment
Pingback: What is Recumbency? Its Role in Healthcare - Science is Life