Table of Contents
INTRODUCTION
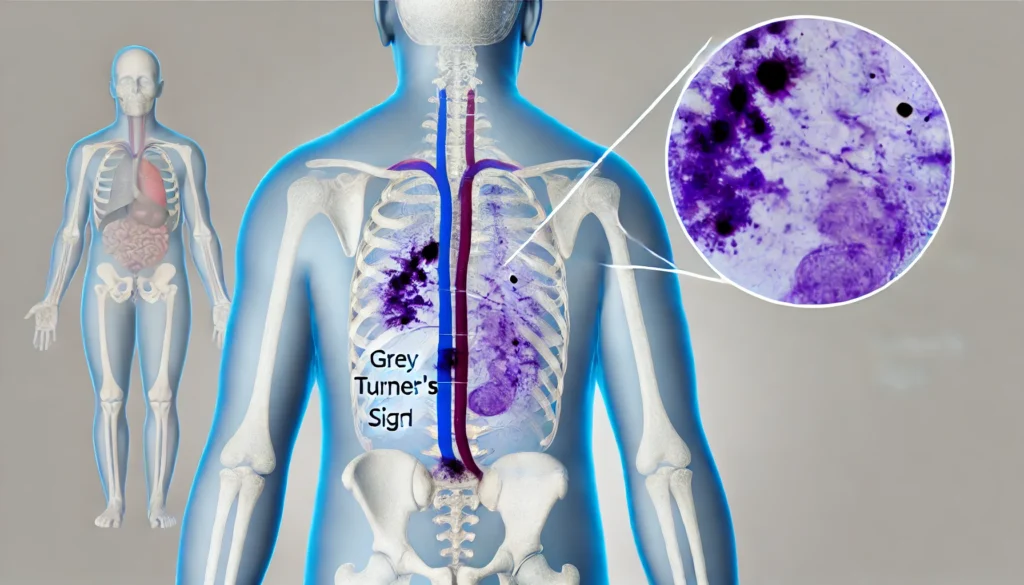
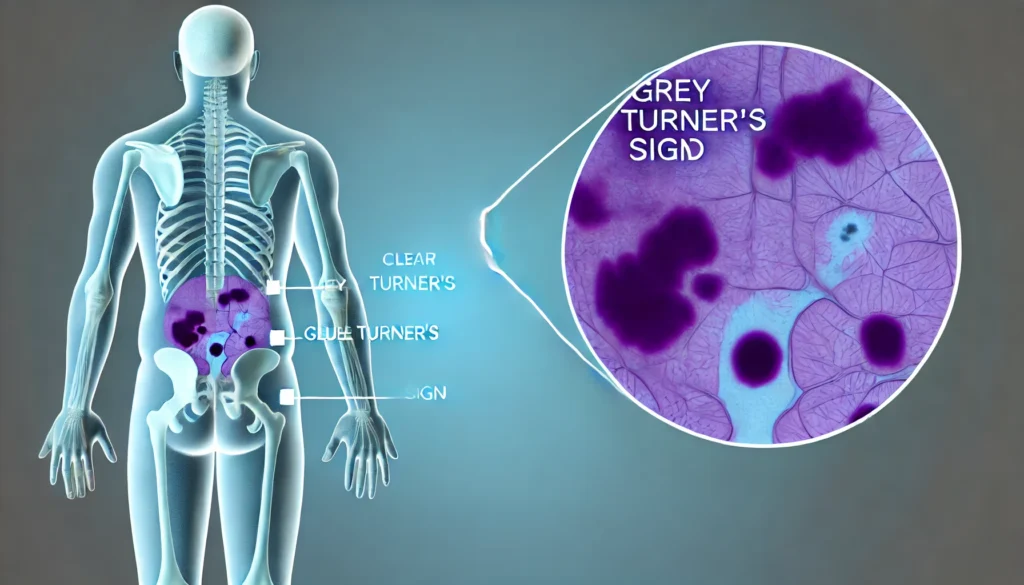
Grey Turner’s Sign is a rare but significant clinical finding first described by the British surgeon George Grey Turner in 1920. It is commonly associated with retroperitoneal hemorrhage or severe pancreatitis. This article provides a comprehensive overview of Grey Turner’s Sign, its etiology, clinical significance, and related conditions.
Definition and Clinical Presentation
Grey Turner’s Sign is characterized by bluish-purple discoloration of the flanks, indicating retroperitoneal hemorrhage. This discoloration typically appears within 24-48 hours and is a critical indicator of internal bleeding (Wright, 2016). The sign is a result of blood tracking subcutaneously from the retroperitoneum to the flanks.

Etiology
Grey Turner’s Sign can result from various serious medical conditions. The most common causes include acute pancreatitis, traumatic injuries, aortic aneurysm, retroperitoneal hemorrhage, and ectopic pregnancy (Dickson & Imrie, 1984; Bem & Bradley, 1998).
Acute Pancreatitis
Acute pancreatitis is one of the most frequent causes of Grey Turner’s Sign. Inflammation of the pancreas can lead to the release of pancreatic enzymes that cause tissue damage and bleeding, spreading to the retroperitoneal area and presenting as Grey Turner’s Sign (Cienfuegos, 2022). This sign often accompanies Cullen’s Sign, which presents as periumbilical ecchymosis.
- Pathophysiology: The activation of pancreatic enzymes causes autodigestion of pancreatic tissue, leading to hemorrhage and necrosis. The spread of the hemorrhage to the retroperitoneal space results in the discoloration observed in Grey Turner’s Sign.
- Clinical Features: Patients with acute pancreatitis typically present with severe abdominal pain, nausea, vomiting, and elevated pancreatic enzymes. The presence of Grey Turner’s Sign indicates a severe form of the disease.
Read:What is Cystolitholapaxy?
Aortic Aneurysm
Aortic aneurysms involve the dilation or rupture of the abdominal aorta, leading to retroperitoneal bleeding. This bleeding can manifest as Grey Turner’s Sign (Kashiwagi, Shimamura & Imamura, 2022). The presence of this sign in a patient with abdominal or back pain should prompt immediate imaging and surgical consultation.
- Pathophysiology: Aortic aneurysms occur due to weakening of the arterial wall, often related to atherosclerosis. A rupture results in massive hemorrhage into the retroperitoneal space.
- Clinical Features: Symptoms include sudden onset of severe abdominal or back pain, hypotension, and shock. Grey Turner’s Sign may be an early indicator of retroperitoneal hemorrhage.
Retroperitoneal Hemorrhage
Retroperitoneal hemorrhage, due to trauma or spontaneous bleeding, is a critical cause of Grey Turner’s Sign. The bleeding into the retroperitoneal space leads to the characteristic flank discoloration. Causes can include anticoagulant therapy, trauma, or ruptured aneurysms.
- Pathophysiology: Retroperitoneal hemorrhage can result from direct trauma, anticoagulant use, or spontaneous vascular rupture. The accumulation of blood in the retroperitoneal space causes the observed discoloration.
- Clinical Features: Symptoms depend on the severity of the hemorrhage and may include flank pain, abdominal distension, and signs of hypovolemic shock.
Ectopic Pregnancy
Ectopic pregnancy, where a fertilized egg implants outside the uterus, can rupture and cause significant internal bleeding. This bleeding may extend to the retroperitoneal space, resulting in Grey Turner’s Sign (Rahbour et al., 2012). This condition is a medical emergency requiring prompt diagnosis and treatment.
- Pathophysiology: Ectopic pregnancy most commonly occurs in the fallopian tube. Rupture leads to massive intra-abdominal bleeding, which can extend to the retroperitoneal space.
- Clinical Features: Symptoms include pelvic pain, vaginal bleeding, and signs of hemodynamic instability. The presence of Grey Turner’s Sign indicates significant internal bleeding.
Clinical Importance
Grey Turner’s Sign is an important diagnostic indicator. Its presence often suggests severe underlying pathology requiring immediate medical attention. Recognizing this sign can lead to timely intervention and better patient outcomes.
Diagnostic Evaluation
When Grey Turner’s Sign is observed, a thorough diagnostic workup is essential. This includes:
- Imaging Studies: CT scans and ultrasounds to identify the source of bleeding or inflammation.
- Laboratory Tests: Blood tests to assess pancreatic enzymes, hematocrit levels, and other relevant markers.
- Clinical Examination: Comprehensive physical examination to correlate with other clinical signs.
Imaging Studies
Imaging plays a crucial role in diagnosing the underlying cause of Grey Turner’s Sign. A CT scan of the abdomen and pelvis is the gold standard for evaluating retroperitoneal structures and identifying hemorrhage, pancreatic pathology, or vascular anomalies.
- CT Scan: Provides detailed images of the abdominal and retroperitoneal structures, identifying the source and extent of hemorrhage.
- Ultrasound: Useful for initial evaluation and in unstable patients where quick bedside imaging is needed.
- MRI: May be used for further evaluation if needed, particularly for soft tissue characterization.
Read: Curette and Endocervical Curettage (ECC)
Laboratory Tests
Laboratory evaluation should include a complete blood count to assess for anemia, serum amylase and lipase levels to diagnose pancreatitis, and coagulation studies to evaluate for bleeding disorders.
- Complete Blood Count (CBC): To check for anemia and overall blood health.
- Serum Amylase and Lipase: Elevated levels indicate pancreatitis.
- Coagulation Profile: To evaluate bleeding tendencies or disorders.
- Electrolytes and Renal Function: To assess overall metabolic status and organ function.
Management and Treatment
The treatment of Grey Turner’s Sign involves addressing the underlying cause:
- Acute Pancreatitis: Supportive care, including fluid resuscitation, pain management, and addressing complications.
- Aortic Aneurysm: Surgical intervention or endovascular repair.
- Retroperitoneal Hemorrhage: Stabilization, blood transfusions, and surgical intervention if necessary.
- Ectopic Pregnancy: Surgical or medical management to terminate the pregnancy and control bleeding.
- Acute Pancreatitis:
- Supportive Care: Fluid resuscitation, pain management, nutritional support.
- Complications: Management of infected necrosis, pseudocysts, and organ failure.
- Long-term Management: Addressing underlying causes such as gallstones or alcohol use.
- Aortic Aneurysm:
- Emergency Surgery: Open repair or endovascular aneurysm repair (EVAR).
- Postoperative Care: Intensive monitoring, blood pressure control, and follow-up imaging.
- Retroperitoneal Hemorrhage:
- Stabilization: Immediate resuscitation with fluids and blood products.
- Surgical Intervention: Depending on the source and severity of the hemorrhage.
- Monitoring and Follow-up: Regular imaging and clinical evaluation.
- Ectopic Pregnancy:
- Medical Management: Methotrexate for early, unruptured ectopic pregnancies.
- Surgical Management: Laparoscopy or laparotomy for ruptured ectopic pregnancies.
- Postoperative Care: Monitoring for hemodynamic stability and recovery.
Case Studies
Case Study 1: Acute Pancreatitis
A 45-year-old male presented with severe abdominal pain radiating to the back. Physical examination revealed Grey Turner’s Sign. Elevated serum amylase and lipase levels confirmed acute pancreatitis. CT imaging showed pancreatic inflammation and retroperitoneal hemorrhage. The patient was managed with supportive care and recovered without surgical intervention (Wright, 2016).
Case Study 2: Ruptured Aortic Aneurysm
A 70-year-old female with a history of hypertension presented with sudden onset of severe back pain and flank discoloration (Grey Turner’s Sign). Imaging revealed a ruptured abdominal aortic aneurysm. Emergency surgical repair was performed, and the patient was stabilized postoperatively (Kashiwagi, Shimamura & Imamura, 2022).
Related Signs and Conditions
Cullen’s Sign
Cullen’s Sign, first described by Thomas Cullen in 1918, is characterized by periumbilical ecchymosis. It is also a sign of intra-abdominal bleeding and is often associated with acute pancreatitis and ruptured ectopic pregnancy (Rahbour et al., 2012).
Differential Diagnosis
When evaluating Grey Turner’s Sign, it is essential to consider other conditions that may present similarly:
- Rectus Sheath Hematoma: Can cause abdominal wall bruising but typically does not extend to the flanks.
- Coagulopathies: Patients on anticoagulation therapy may present with spontaneous bleeding and bruising.
- Trauma: Direct trauma to the abdomen or flanks can cause localized ecchymosis.
Prognosis
The prognosis of Grey Turner’s Sign depends on the underlying condition. Acute pancreatitis has a variable prognosis based on severity and complications, while ruptured aortic aneurysm and ectopic pregnancy can be life-threatening without prompt intervention.
- Acute Pancreatitis: Prognosis varies with the severity of the inflammation and complications. Early intervention and management of complications improve outcomes.
- Aortic Aneurysm: Prognosis is poor without immediate surgical intervention. Survival rates increase significantly with timely repair.
- Retroperitoneal Hemorrhage: Prognosis depends on the cause and extent of the hemorrhage. Prompt stabilization and treatment are crucial.
- Ectopic Pregnancy: Prognosis is good with early detection and treatment. Ruptured ectopic pregnancies require immediate intervention to prevent mortality.
Read:What is Trabeculae Carnea?
Prevention and Awareness
Awareness of Grey Turner’s Sign and its implications is crucial for healthcare providers. Early recognition and diagnosis can significantly impact patient outcomes. Preventive measures include managing risk factors for acute pancreatitis, such as alcohol consumption and gallstone disease, and monitoring patients with known aneurysms.
- Education: Training healthcare providers to recognize Grey Turner’s Sign and its implications.
- Public Awareness: Educating at-risk populations about the signs and symptoms of underlying conditions such as pancreatitis and aortic aneurysm.
- Regular Screenings: For individuals with risk factors such as atherosclerosis or a family history of aneurysms.
Tables and Figures
| Condition | Key Features |
| Acute Pancreatitis | Elevated pancreatic enzymes, abdominal pain |
| Aortic Aneurysm | Pulsatile abdominal mass, hypotension |
| Retroperitoneal Hemorrhage | Trauma history, shock |
| Ectopic Pregnancy | Positive pregnancy test, pelvic pain |
| Test | Purpose |
| Complete Blood Count (CBC) | Assess for anemia and overall blood health |
| Serum Amylase and Lipase | Diagnose acute pancreatitis |
| Coagulation Profile | Evaluate bleeding disorders |
| Electrolytes and Renal Function | Assess overall metabolic status and organ function |
Conclusion
Grey Turner’s Sign is a critical clinical finding indicating serious underlying conditions such as acute pancreatitis, aortic aneurysm, and retroperitoneal hemorrhage. Early recognition and appropriate management are essential for improving patient outcomes. This comprehensive overview highlights the importance of understanding Grey Turner’s Sign in clinical practice.
References
- Wright WF. Cullen Sign and Grey Turner Sign Revisited. J Am Osteopath Assoc. 2016;116(6):398-401.
- Dickson AP, Imrie CW. The incidence of body wall ecchymosis in acute pancreatitis. Surg Gynecol Obstet. 1984;159(4):343–7.
- Bem J, Bradley EL. Subcutaneous manifestations of severe acute pancreatitis.Pancreas. 1998;16(4):551-5.
- Rahbour G, Ullah MR, Yassin N, Thomas GP. Cullen’s sign – case report with a review of the literature. Int J Surg Case Rep. 2012;3(5):143-6.
- Cienfuegos JA, Valentí V, Rotellar F. Acute pancreatitis: an opportunity for gastroenterology hospitalists? Rev Esp Enfermedades Dig. 2022;114:73-75.
- Kashiwagi R, Shimamura Y, Imamura K. Uncommon etiology of Cullen’s sign and Grey Turner sign.J Gen Fam Med. 2022;23(4):282-3.


